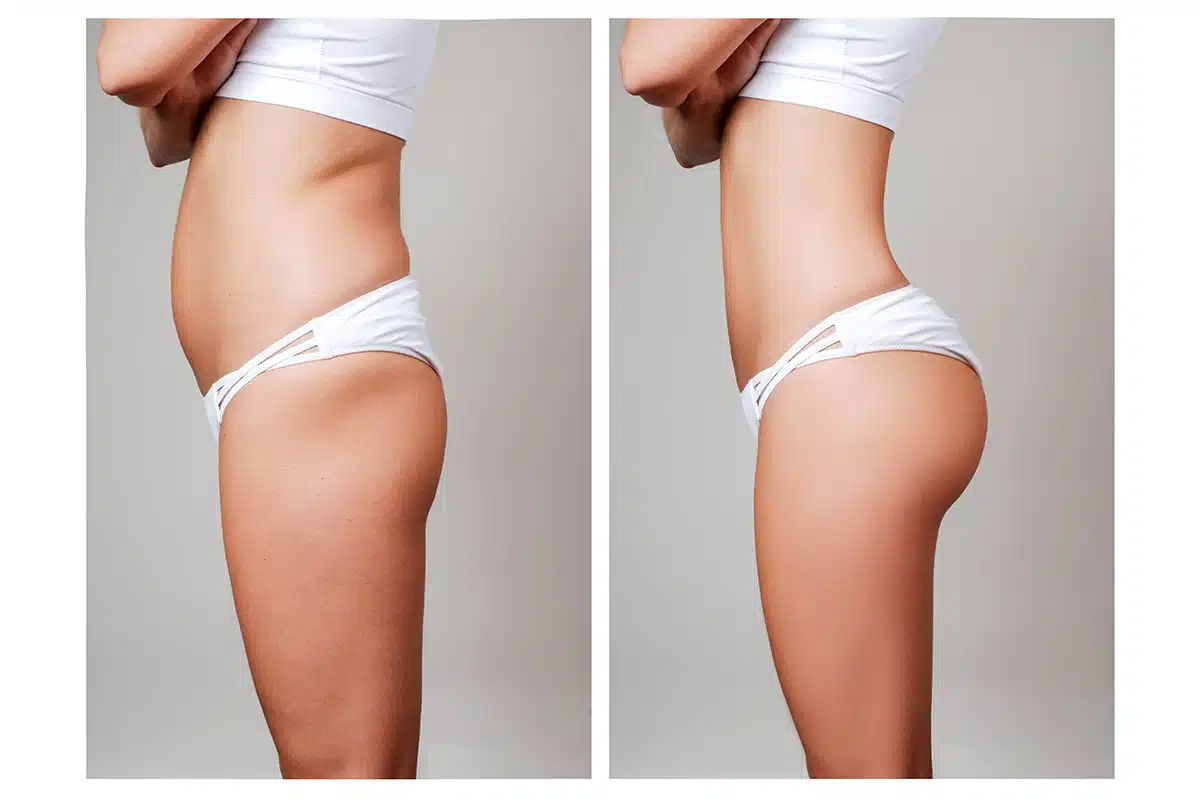
The decision to enhance the gluteal contour using injectable materials—whether it involves utilizing biostimulatory agents like poly-L-lactic acid (PLLA), large-volume hyaluronic acid (HA) fillers, or other off-label synthetic compounds—is often driven by the appeal of minimal downtime compared to surgical alternatives like the Brazilian Butt Lift (BBL). However, describing the post-procedure period merely as “minimal downtime” fundamentally oversimplifies the actual recovery process, which is a nuanced and critical phase directly impacting the final aesthetic outcome and long-term safety. Unlike the surgical recovery that focuses on healing from incisions and trauma, recovery after butt injections centers on managing swelling, optimizing material integration, and strictly adhering to protocols designed to prevent migration or complications of the injected product. A successful result is less dependent on the immediate procedure and more dependent on the patient’s diligent compliance with specific restrictions on sitting, exercise, and pressure for the weeks and months following the treatment. Understanding the distinction between the immediate post-injection period and the long-term integration phase is essential for anyone considering this non-surgical route.
Recovery After Butt Injections Centers on Managing Swelling
The initial phase of recovery begins immediately after the last injection, and its most prominent feature is swelling. Recovery after butt injections centers on managing swelling, which is an inevitable biological response to the trauma of the needles and the volume of the injected material. This swelling is usually generalized across the treated area and can make the buttocks appear larger than the final anticipated size. This initial volume is often misleading and patients must be prepared for a gradual reduction as the swelling subsides over the first week or two. In addition to swelling, patients will typically experience localized soreness, tenderness, and bruising at the multiple injection sites. The intensity of this discomfort is generally mild to moderate and is usually managed effectively with over-the-counter pain relievers. The severity and duration of the bruising are highly individual, depending on the patient’s propensity to bruise and the specific technique employed by the practitioner, but the presence of these immediate, temporary side effects is a normal part of the process and must not be confused with complications.
The Most Critical Restriction Involves Avoiding Direct, Sustained Pressure
The paramount concern immediately following gluteal injections is ensuring that the highly viscous or volume-adding materials remain precisely where the practitioner placed them. Therefore, the most critical restriction involves avoiding direct, sustained pressure on the buttocks. This is the single most defining difference between this recovery and nearly any other aesthetic procedure. While surgical BBL patients also avoid sitting to protect the transferred fat, injection patients avoid it to prevent the migration or displacement of the filler material before it has stabilized or integrated into the surrounding tissue. Patients are typically instructed to lie on their stomach or side, even while sleeping, for a period that can range from one to three weeks, depending on the volume and type of material used. When sitting is absolutely necessary, the use of specialized cushions or “donut” pillows that offload pressure from the injected area onto the back of the thighs is mandatory. Failure to adhere strictly to this protocol can ruin the contouring effect and lead to palpable lumps or asymmetry.
Physical Activity Must Be Reduced to Prevent Displacement
For individuals with active lifestyles, the required modifications to physical activity present a significant adjustment during the recovery period. Physical activity must be reduced to prevent displacement of the product, particularly during the first few weeks. High-impact exercises, activities that put repetitive stress on the gluteal muscles (like squats, running, or cycling), and those that require constant muscle contraction must be strictly avoided. Intense muscle movement, especially during the crucial initial integration phase, can essentially “squeeze” the newly placed material, altering the intended contour and potentially forcing the filler to migrate away from the deep subcutaneous plane where it was strategically placed. Most practitioners advise a return to light walking only, with a gradual, staged reintroduction of more strenuous lower-body exercise only after receiving explicit clearance, which is usually weeks after the initial procedure.
Strict Management Is Required During the Early Integration Phase
The recovery process must be differentiated based on the type of material injected, particularly between volumizing fillers and biostimulators. Volumizing fillers, such as HA products, require strict management during the early integration phase because the primary risk is migration before the product’s gel matrix stabilizes within the tissue. Biostimulators, such as PLLA, present a unique set of post-procedure requirements focused on promoting the desired biological response. For biostimulators, strict management is required during the early integration phase to ensure even distribution and uniform collagen synthesis. Patients are often instructed to massage the injected areas vigorously several times a day for a week or more. This massage is critical to break up potential clumps of the material and ensure that the subsequent collagen growth creates a smooth, uniform surface rather than palpable nodules.
The Process of Collagen Synthesis Takes Several Months
A crucial psychological component of recovery from biostimulatory injections is patience, as the aesthetic results are significantly delayed. Unlike volumizing HA fillers that provide immediate bulk (though obscured by swelling), biostimulators achieve their effect over time. The process of collagen synthesis takes several months to complete. After the initial post-procedure swelling resolves, the patient may see little change for many weeks, which can be discouraging if they are not properly prepared. The aesthetic improvement—the lifting, firming, and subtle increase in volume—begins to manifest gradually, often three to six months after the treatment, as the newly created collagen provides structural support. This delayed gratification necessitates a different mindset from the patient, moving from an expectation of immediate results to a commitment to a slow, biological process.
The Possibility of Palpable Nodules or Lumps Must Be Discussed
Regardless of the type of filler used, the possibility of palpable nodules or lumps must be discussed as part of the informed consent and recovery plan. While a skilled practitioner minimizes this risk through proper injection technique and depth, the body’s reaction to any foreign material can sometimes involve the formation of granulomas or localized encapsulation. In the case of biostimulators, insufficient post-treatment massage can lead to the formation of visible or palpable nodules where the concentrated material triggered too much localized collagen growth. For volumizing fillers, the risk involves the product clumping or being displaced. Managing this complication often involves further intervention, such as steroid injections to break down the granuloma or hyaluronidase to dissolve HA fillers, underscoring the necessity of strict adherence to all post-procedure care protocols designed to prevent this outcome.
Long-Term Surveillance and Touch-Ups Are a Standard Expectation
Because the results of non-surgical butt injections are not permanent—whether due to the natural absorption of HA or the gradual turnover of collagen stimulated by PLLA—the recovery process transitions into a phase of maintenance. Long-term surveillance and touch-ups are a standard expectation of this route of gluteal enhancement. Patients must be prepared for the fact that the volume and contour will gradually diminish over time, often necessitating a return for repeat treatments every 12 to 24 months, depending on the material and individual metabolism. This continuous cycle of treatment and recovery distinguishes the non-surgical method from the surgical BBL, where the surviving fat cells are permanent. This commitment to ongoing maintenance needs to be factored into the patient’s long-term financial and time budget.
The True Measure of Safety and Efficacy Is the Skill of the Practitioner
It is impossible to discuss recovery without acknowledging the pivotal role of the injector. The true measure of safety and efficacy is the skill of the practitioner performing the butt injections. This area of aesthetic medicine, particularly involving large volumes of product, is not regulated uniformly, and complications often arise from practitioners lacking the advanced anatomical knowledge to inject safely into the correct planes, avoiding major nerves and blood vessels. A recovery that involves extreme, unmanaged pain, signs of vascular compromise (such as marbled, pale, or unusually cold skin), or persistent, dramatic swelling beyond the first week should trigger immediate contact with the practitioner. The patient’s recovery is heavily mitigated by the initial procedure’s quality, making the choice of a highly trained, board-certified professional the most crucial preventative measure against a complicated recovery.
The Psychological Aspect of Recovery Should Not Be Overlooked
Beyond the physical limitations, the psychological aspect of recovery should not be overlooked, particularly concerning the delayed nature of the results for biostimulators. The inability to see an immediate, dramatic change can lead to anxiety, self-doubt, and the premature conclusion that the procedure has failed. Furthermore, the restrictions on sitting and exercise—activities central to many people’s daily lives—can contribute to feelings of isolation or frustration. Managing this psychological impact requires the practitioner to provide clear, phased timelines for physical restrictions and expected aesthetic milestones, constantly reinforcing the message that the patient’s adherence to the protocol is what drives the final success, fostering compliance through education and psychological support.
Nutritional Support for Collagen Production Is Recommended
To actively support the body’s repair processes and maximize the benefit of biostimulators, recovery protocols are increasingly incorporating internal support strategies. Nutritional support for collagen production is recommended to optimize the biological response to the injected material. This often involves ensuring the patient has an adequate intake of protein, Vitamin C, zinc, and copper—essential co-factors in the body’s natural collagen synthesis pathways. While the body will attempt to produce collagen regardless, optimizing these nutritional building blocks can theoretically enhance the quality and quantity of the new collagen formed around the PLLA particles, leading to a potentially better and more durable final contour. This integration of internal wellness into the recovery plan marks a comprehensive, modern approach to non-surgical aesthetic results.
